Analysis of Prior Authorization Trends in Medicare Advantage for 2022
Analysis of Prior Authorization Trends
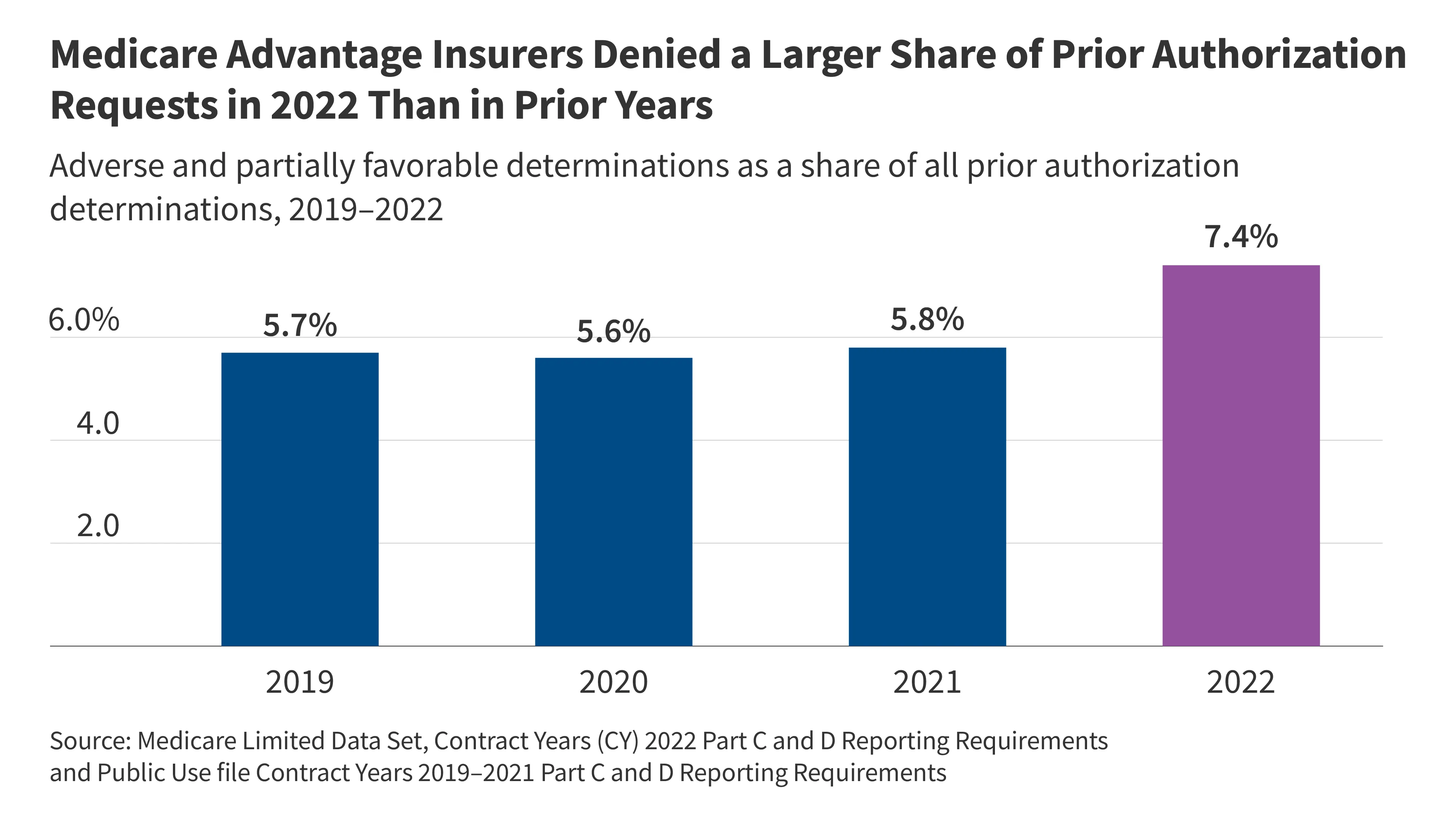
In 2022, Medicare Advantage plans recorded a staggering 46.2 million requests for prior authorization.
Denial Rates and Appeals
Of these, 3.4 million requests were denied, equating to a denial rate of 7.4%. This indicates significant volume within the system.
Variation Among Insurers
- The volume of requests varies by insurer.
- Denial rates are not uniform across all providers.
- Appeal rates and the proportion of successful appeals also fluctuate.
Conclusion
These findings suggest a complex landscape in Medicare Advantage regarding prior authorizations. It highlights the importance for both providers and enrollees to be informed and proactive in managing prior authorization requests.
This article was prepared using information from open sources in accordance with the principles of Ethical Policy. The editorial team is not responsible for absolute accuracy, as it relies on data from the sources referenced.